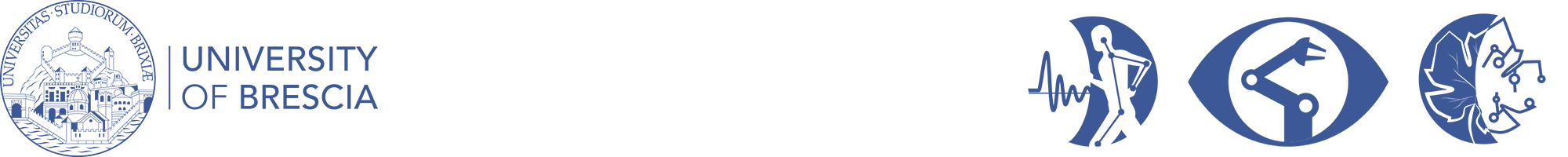
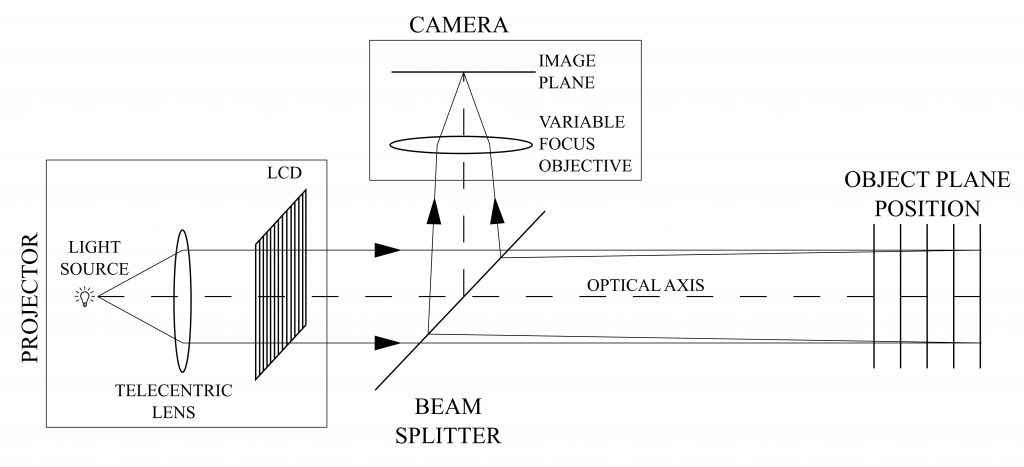
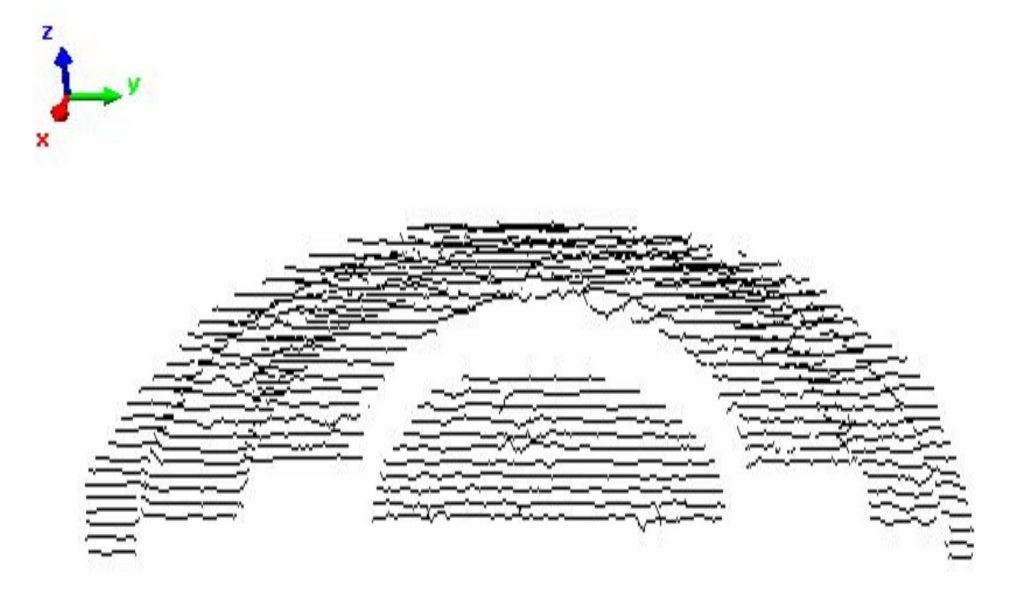
A novel Depth From Defocus (DFD) measurement system is has been developed. Here the extension of the measurement range is performed using an emergent technology based on liquid lenses. A suitable set of different focal lengths, obtained by properly changing the liquid lens supply voltage, provides multiple camera settings without duplicating the system elements or using moving parts.
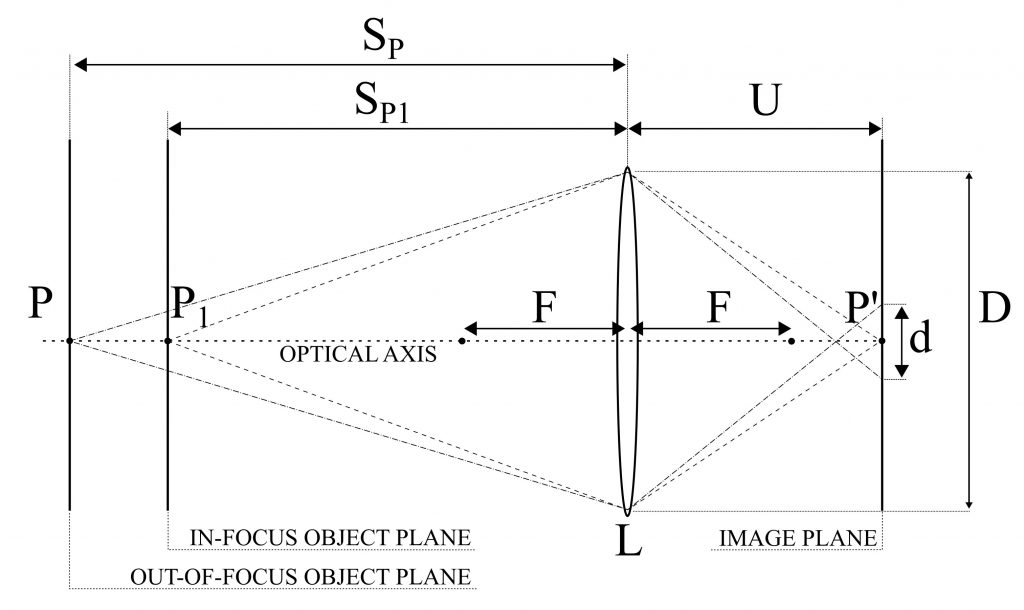
A simple and compact setup, with a single camera/illuminator coaxial assembly is obtained. The measurement is based on an active DFD technique using modulation measurement profilometry(MMP) for the estimation of the contrast at each image point as a function of the depth range.
A suitable combination of multiple contrast curves, each one derived at a specific focal length, is proposed to extend the measurement range and to improve the measurement performances with respect to the state of the art.
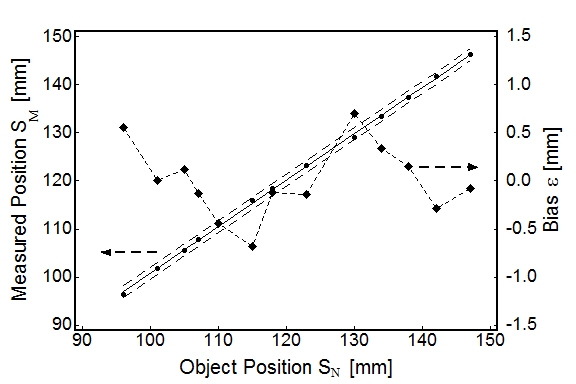
The system measurement errors are 0.53 mm over an extended measurement depth range of 135 mm, corresponding to 0.39 % of the depth range, resulting in an improved performance with respect to the state of the art DFD systems, for which typical values are in the 0.7-1.6 % of the depth range.
Related publications
Pasinetti, S.; Bodini, I.; Lancini, M.; Docchio, F.; Sansoni, G. “A Depth From Defocus Measurement System Using a Liquid Lens Objective for Extended Depth Range“, IEEE Transactions on Instrumentation and Measurement, Vol 66, no. 3, pp. 441-450. 2017